You will be transferred to the Electrophysiology Laboratory (EP lab) from your ward. Usually before leaving your ward your groin will be shaved.
The EP lab has a patient table, X-Ray tube, ECG monitors and various equipment. The staff in the lab will all be dressed in hospital theater clothes and during the procedure will be wearing hats and masks.
Many ECG monitoring electrodes will be attached to your chest area and patches to your chest and back. These patches may momentarily feel cool on your skin.
A nurse or doctor will insert an intravenous line usually into the back of your hand. This is needed as a reliable way to give you medications during the study without further injections. You will also be given further sedation if and as required. You will also have a blood-pressure cuff attached to your arm that will automatically inflate at various times throughout the procedure.
An anesthetist will be present for many procedures. The procedure may be performed under local anaesthetic with sedative medication or under full general anaesthetic. This will be discussed with you before the procedure.
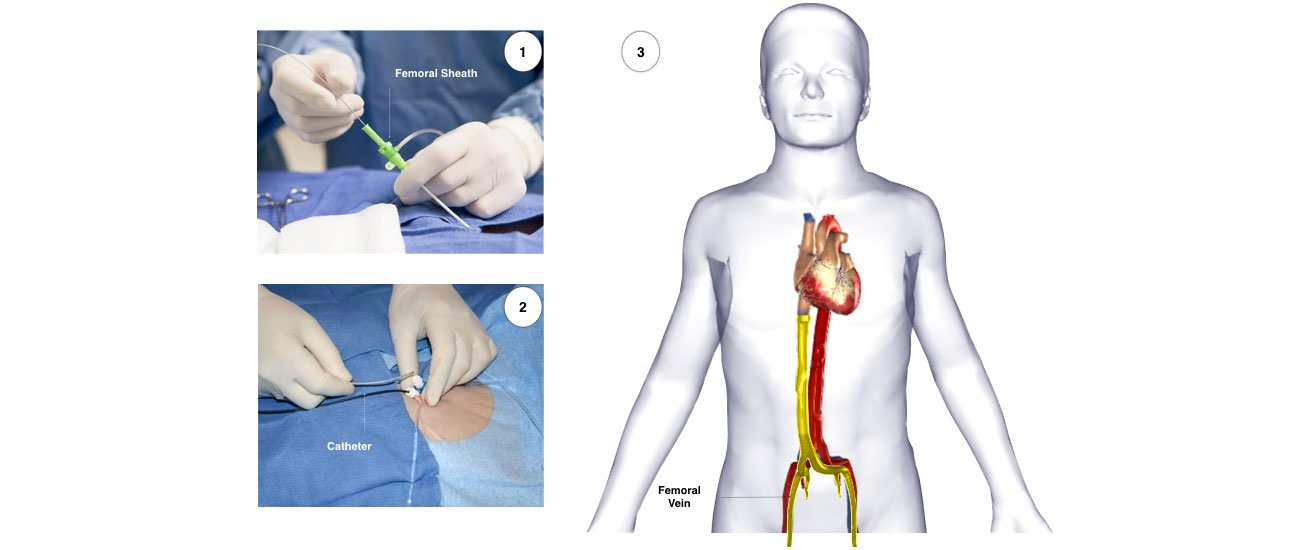
If the procedure is performed under local anaesthetic, the doctor will inject the anaesthetic to the area in the groin where the catheters are to be placed. After that, you may feel pressure as the doctor inserts the catheters but you should not feel pain. If there is any discomfort you should tell the nursing staff so that more local anaesthetic and sedative medication can be given. Occasionally it is also necessary to place a catheter in a vein in the side of the neck.
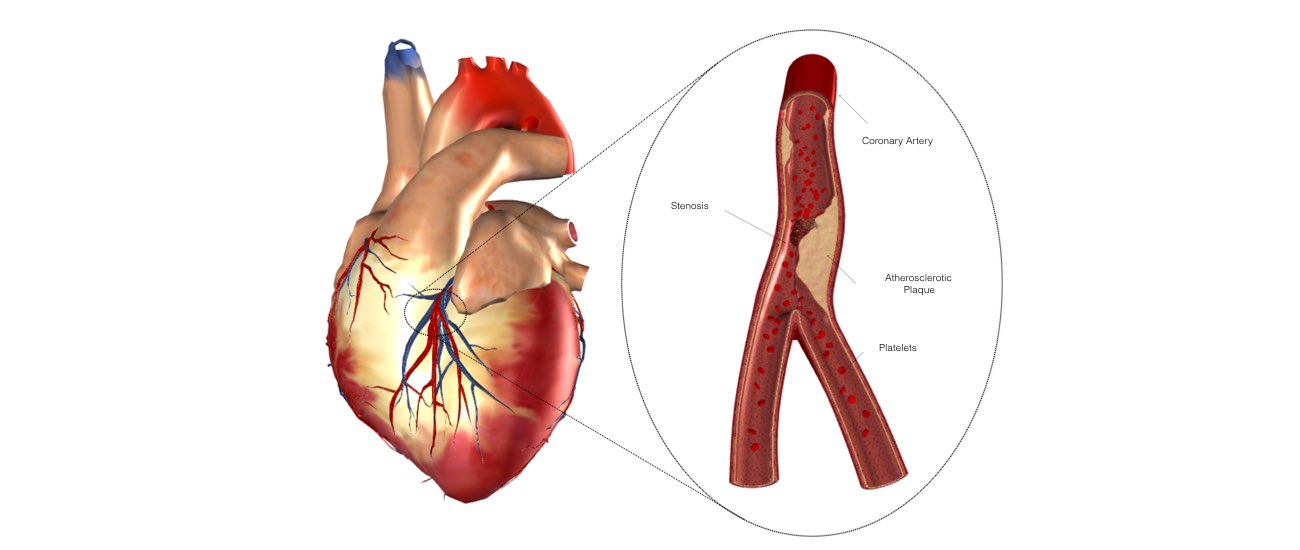
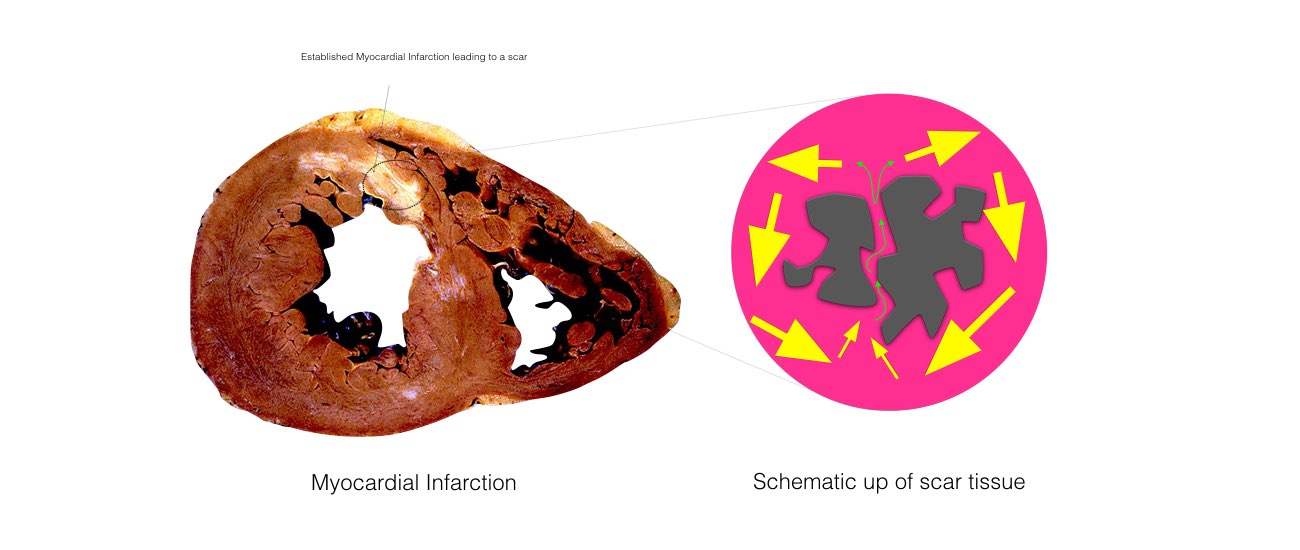
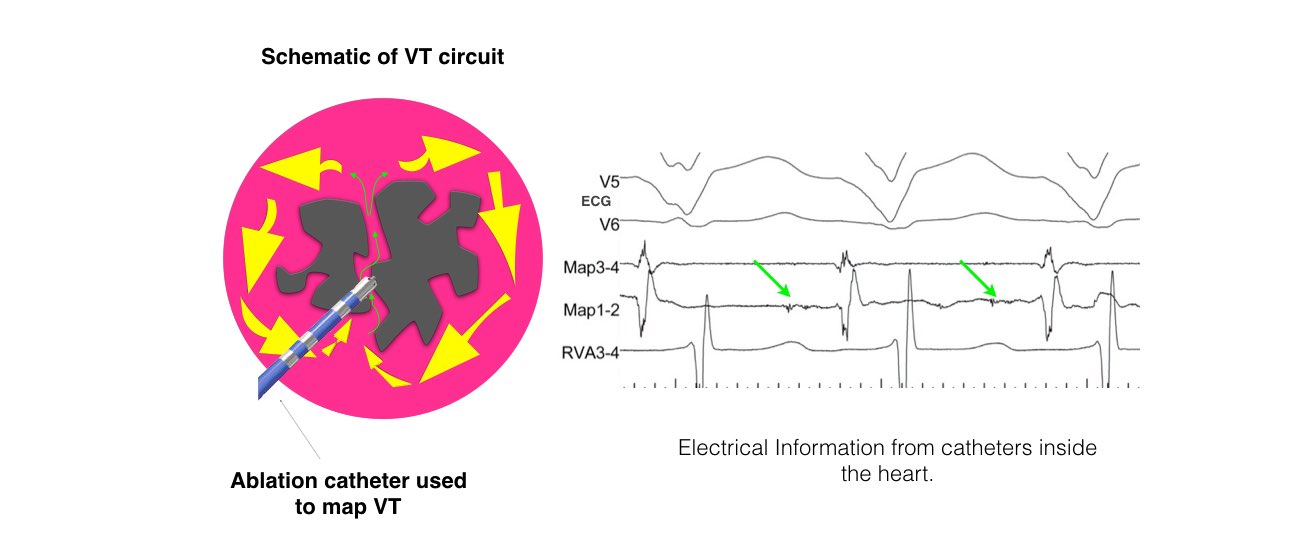
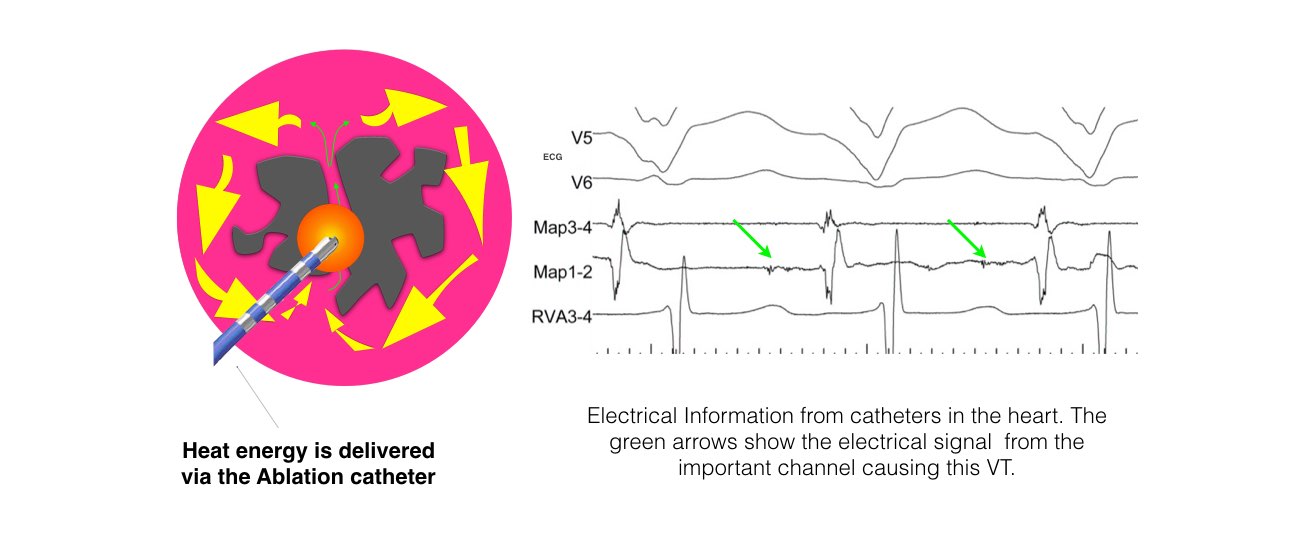
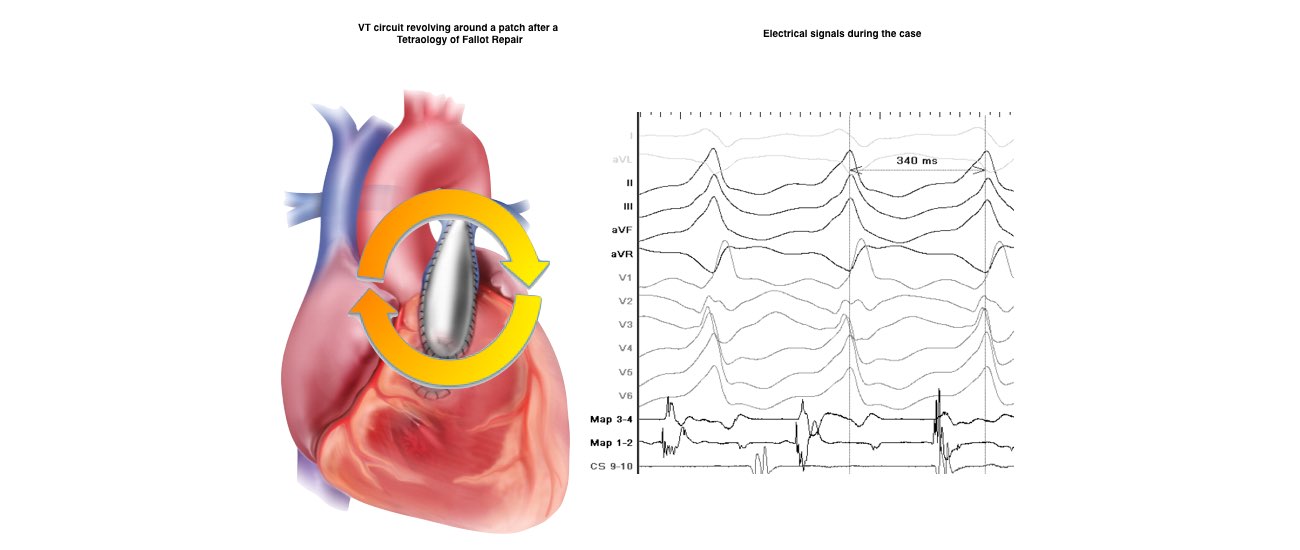
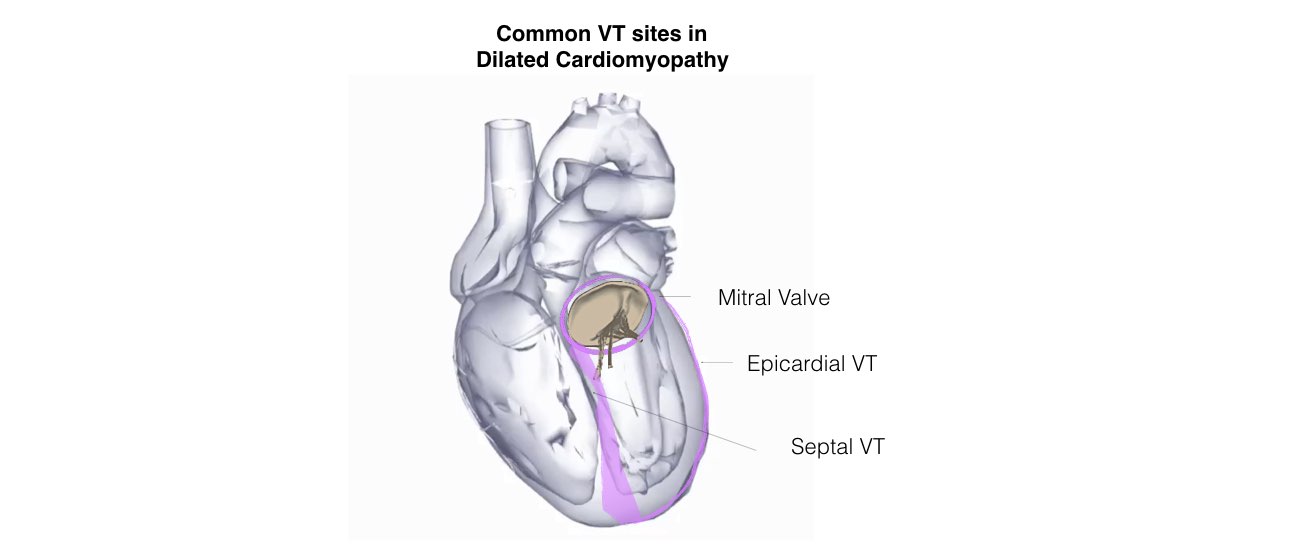
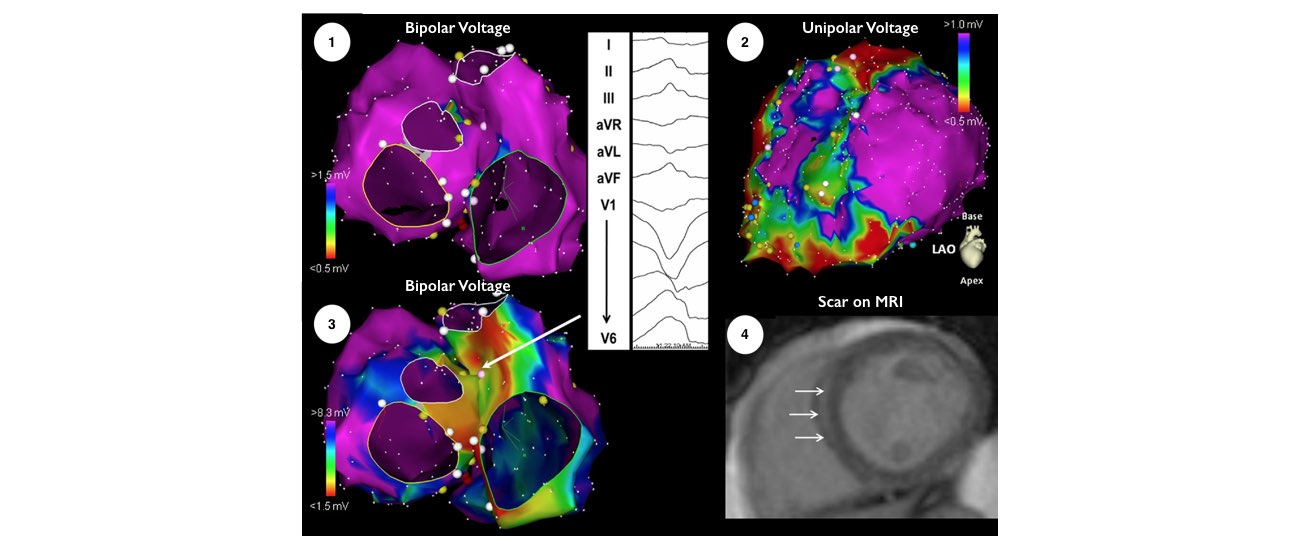
The catheters are positioned in your heart using X-Ray guidance. Once the catheters are in place you may feel your heart being stimulated and usually your abnormal heart rhythm will be induced. We will use a three-dimensional computer mapping system to guide the ablation procedure. This will help us move the catheters in your heart without the need for X-rays and also help us create an electrical map of the VT circuits. When the VT circuits have been identified and the abnormal tissue localized, the radiofrequency ablation will be applied to this spot. This may cause a transient warm discomfort in the chest. Radiofrequency ablation procedures are lengthy and the average duration is approximately 3 to 4 hours.
The catheters are inserted through intravenous ports, or sheaths, placed in the veins in the groin and sometimes through a vein on the side of the neck. To access the left ventricle, a needle may be used to create a small puncture in the wall between the right and left sides of the heart under ultrasound guidance (called transseptal catheterization). Alternatively, a catheter can be inserted into the heart through an artery in the groin (similar to heart catheterization procedures). The ablation catheter is moved around the ventricle, and a virtual 3-dimensional image of the heart is created with a computer mapping system that acts like a navigation system . The location of the catheter is determined by use of fluoroscopy (x-ray) and this mapping system. Typically, the procedure lasts from 3 to 6 hours.
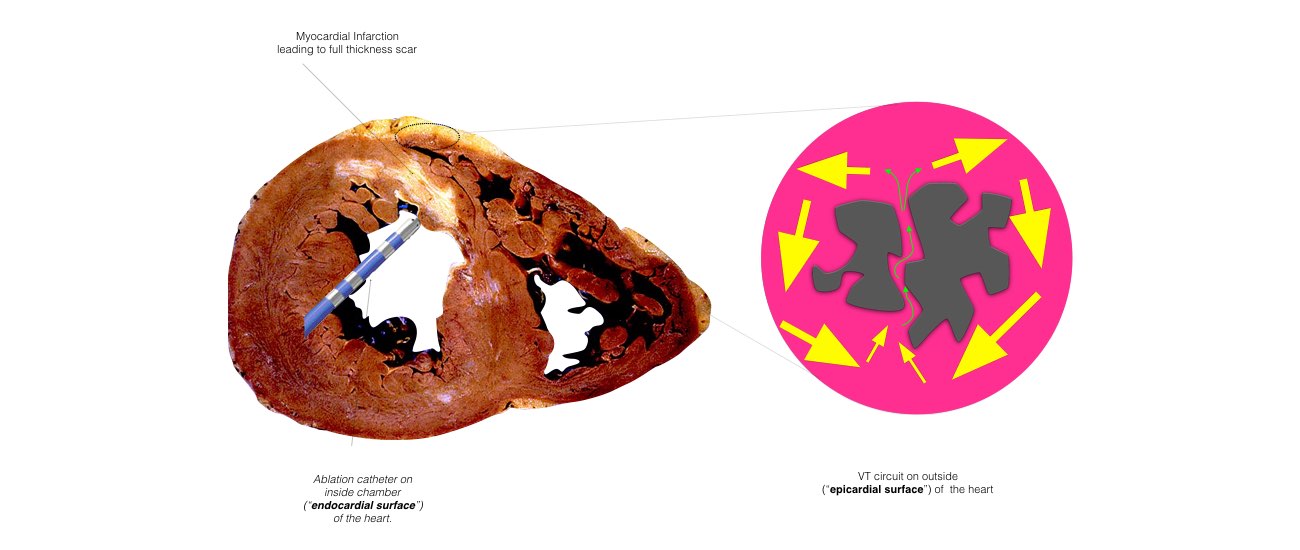
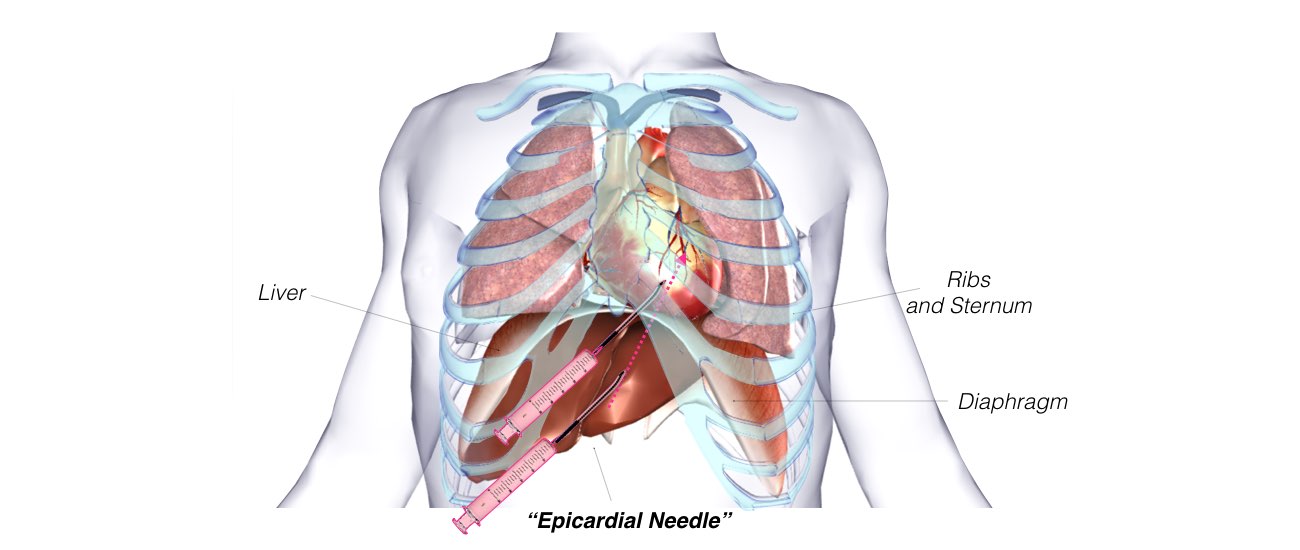
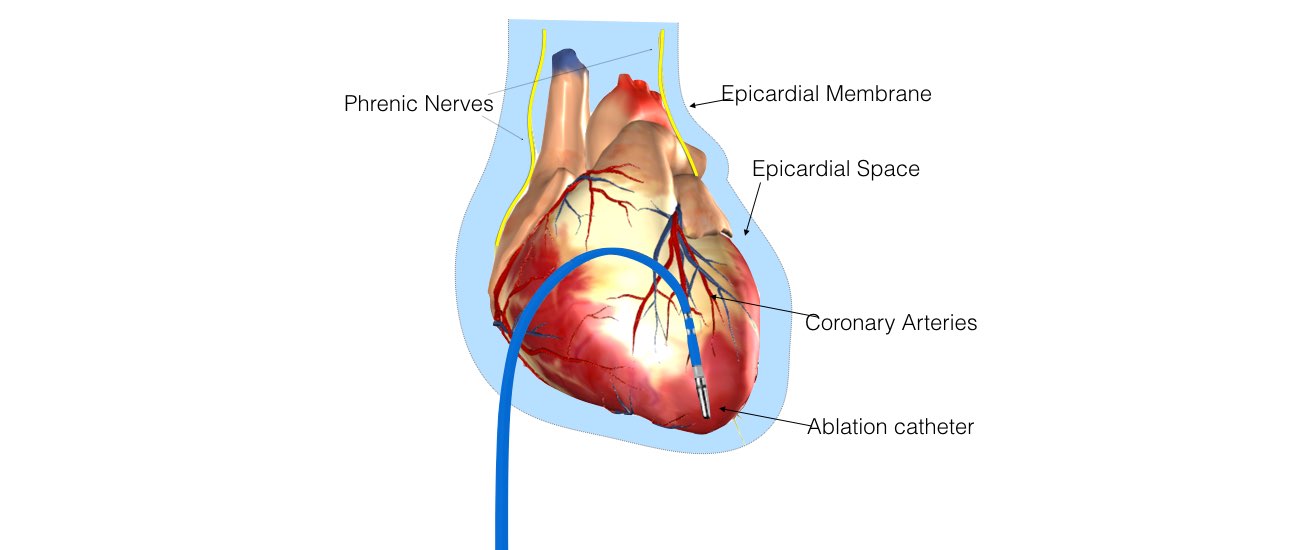
In some instances, the physician determines that the VT may originate from a circuit on the outer surface of the heart, or epicardium. If this is the case, a puncture into the sac, or pericardium, around the heart is performed just beneath the breastbone. This enables the ablation catheter to be inserted and maneuvered within the pericardium to determine whether the VT originates there. If a patient has a previous history of open heart surgery, a small surgical incision may be necessary to access the pericardium because of the presence of scar tissue, which can make the pericardium stick to the heart. These procedures to access the epicardium are usually performed at highly experienced centers.
Afterward, the catheters are removed, but the sheaths are left in until the blood thinner wears off. Typically, this requires the patient to lie still for several hours to prevent bleeding from the puncture sites. Slight discomfort and bruising in the groin area can occur, and some patients experience self-limited mild chest pain resulting from inflammation caused by the ablation lesions. When the procedure is successful, antiarrhythmic medications may be stopped at the discretion of the physician.