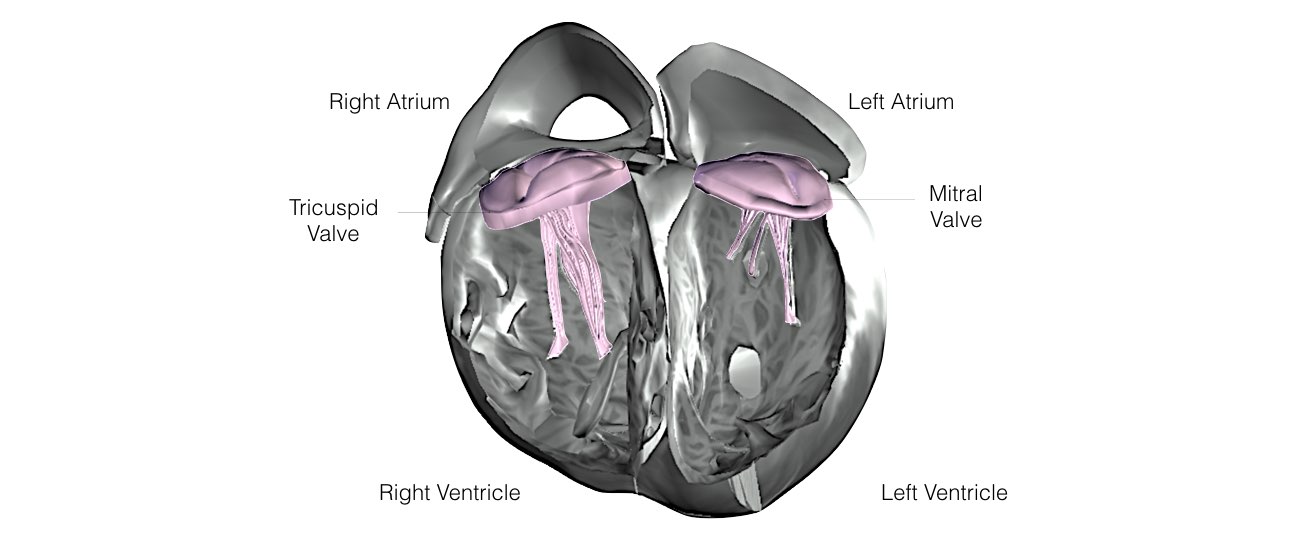
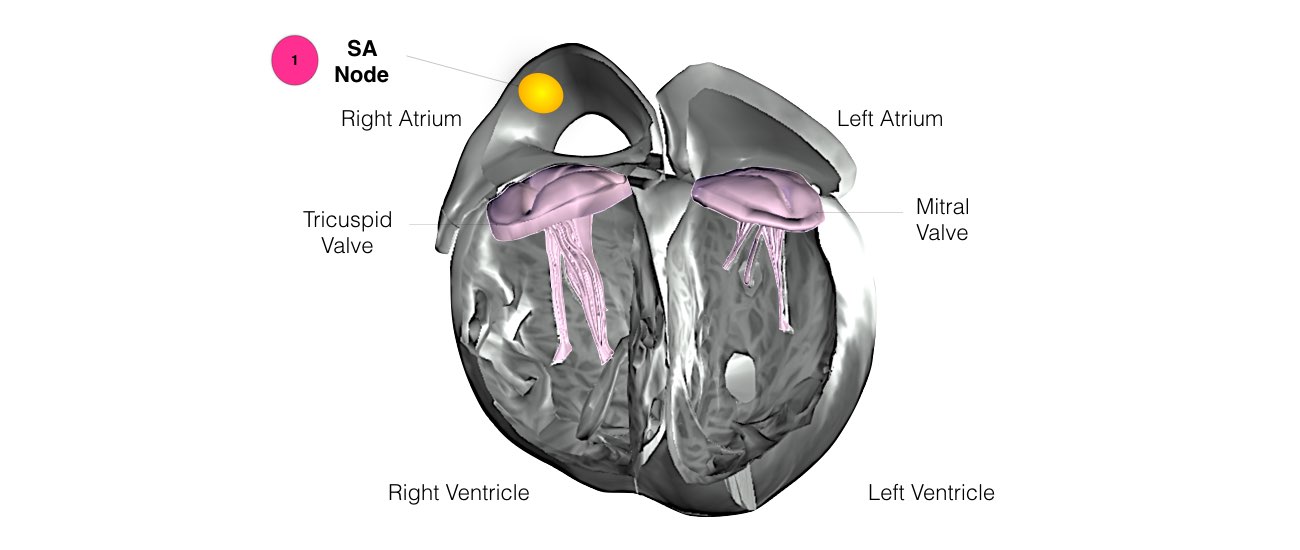
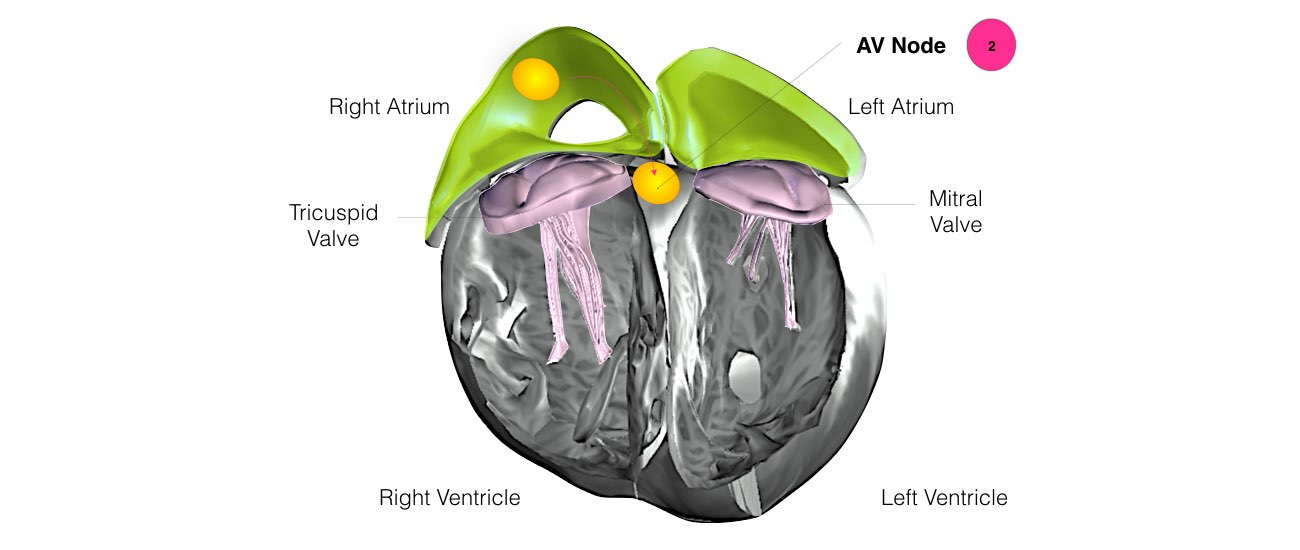
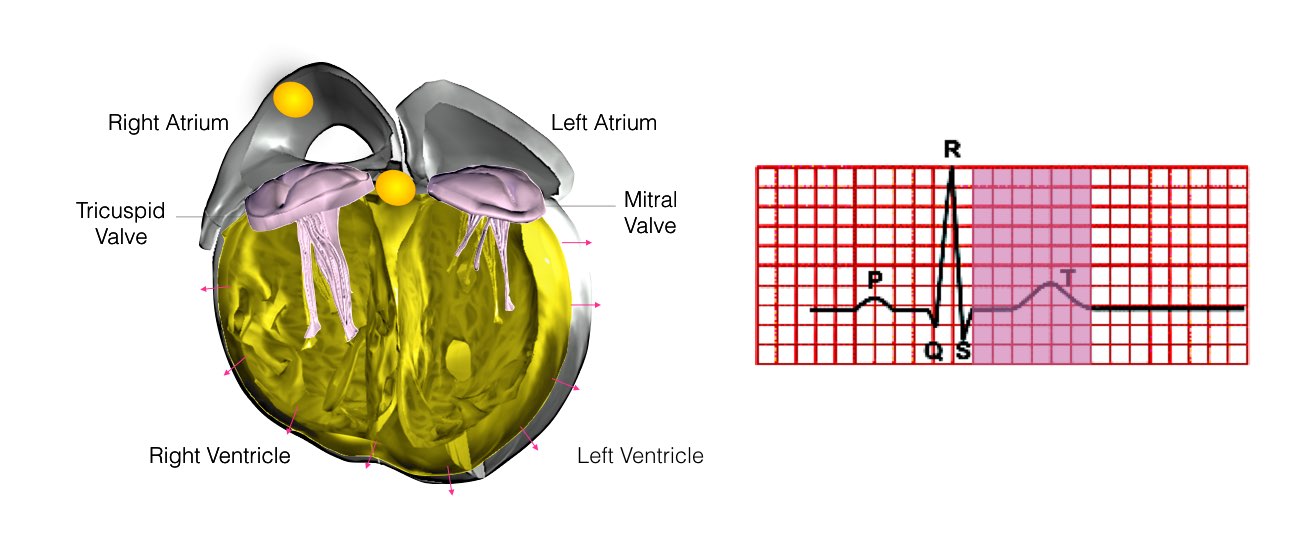
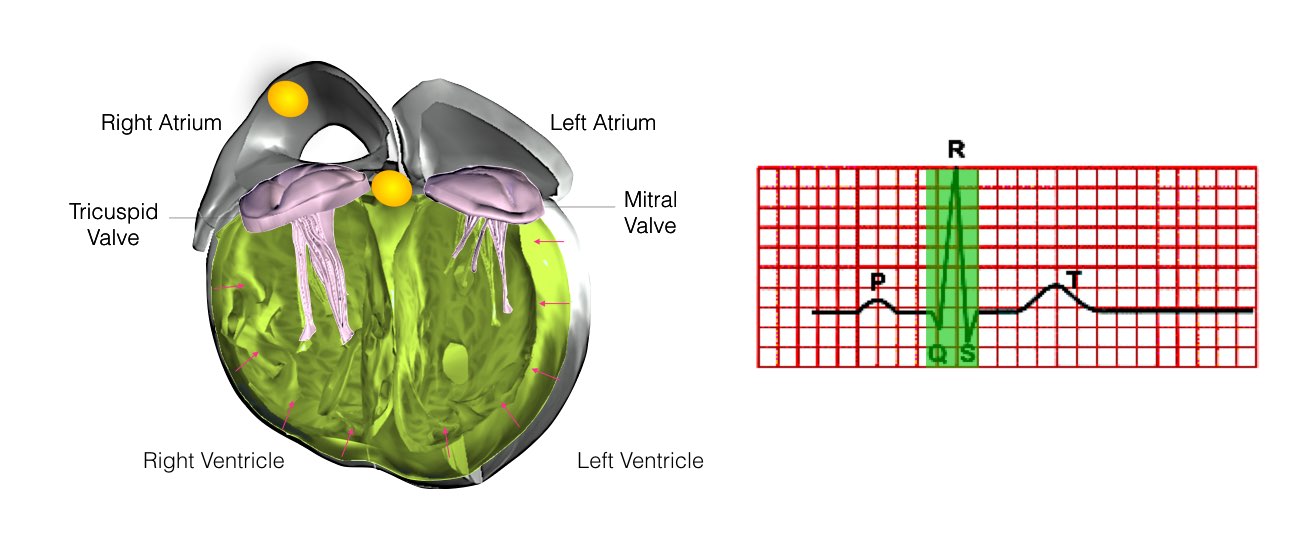
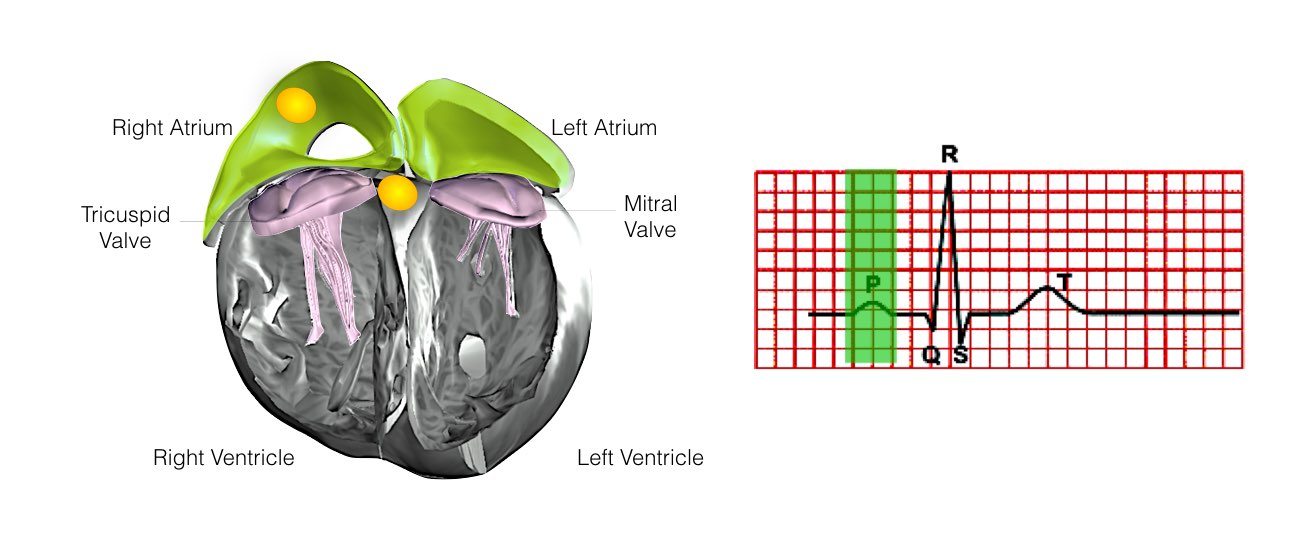
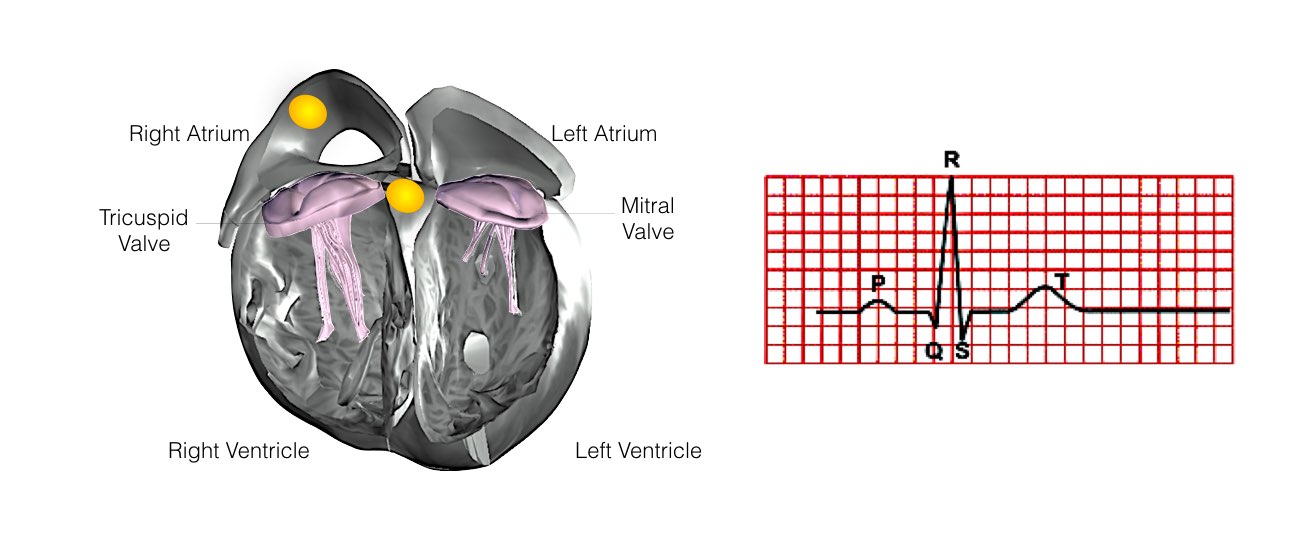
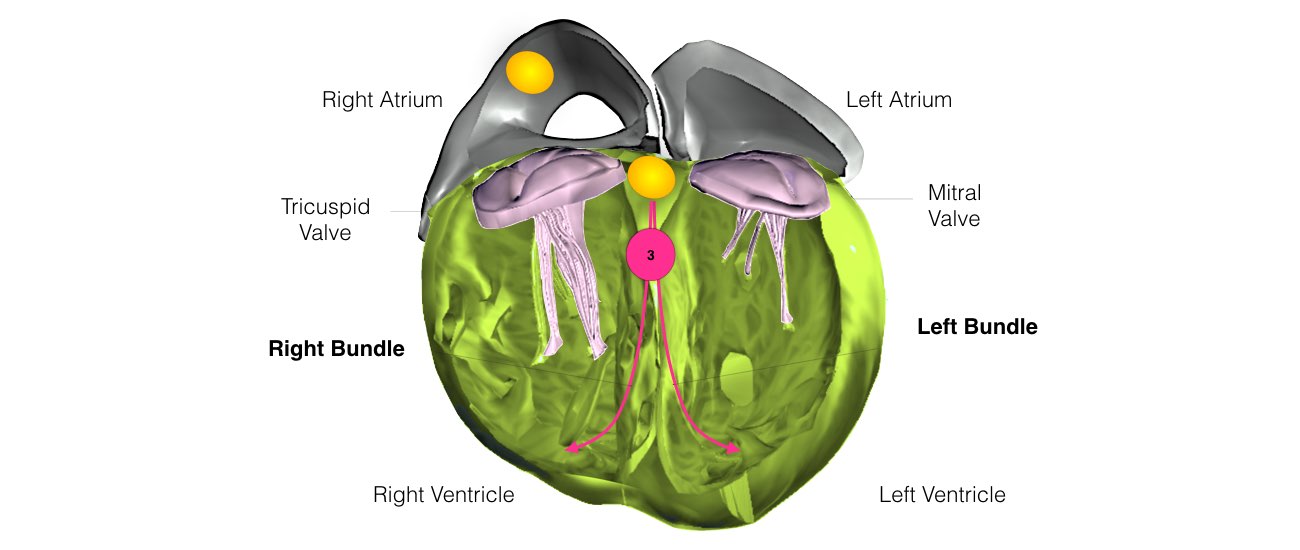
An EP study is a low-risk procedure that has been performed in major medical centres for many years. The EP study makes it possible to study your abnormal heart rhythm under controlled conditions and diagnose your particular problem. (In this procedure, one or more thin, flexible wires, called catheters, are inserted into a blood vessel usually the groin and guided into the heart). Each catheter has two or more electrodes to measure the heart’s electrical signals as they travel from one chamber to another. An EP study is usually done under local anaesthesia.
An EP Study offers more detailed information about the heart’s electrical activity than many other noninvasive tests because electrodes are placed directly on heart tissue. EP studies are done to diagnose your cardiac rhythm abnormality, especially in a patient with palpitation or unexplained loss of consciousness, to help determine the best treatment. EP study allows the Electrophysiologist to determine the specific location of an arrhythmia and, often, to correct it during the same procedure.